Posted by: Focal Point Vision in Blog

The cornea is a vital part of the eye that serves as its protective front window, and when problems arise, accurate diagnosis is crucial for preserving your vision. If you think you may have a corneal condition, the first step is to schedule a comprehensive eye exam with an eye doctor.
They’ll perform a variety of tests to diagnose your condition, then create a custom treatment plan for you based on the results. Keep reading to learn more about how eye doctors test for corneal conditions and how you can prepare for your comprehensive eye exam.
Common Corneal Conditions
The cornea is the clear, dome-shaped tissue covering the front of your eye. It plays a vital role in focusing light onto your retina and protecting your eye from debris and infection.
When corneal problems develop, they can significantly impact your vision and comfort. Common corneal conditions include keratoconus, corneal dystrophies, keratitis, corneal ulcers, pterygium, and corneal abrasions.
Each condition requires specific diagnostic approaches to ensure accurate identification and appropriate treatment planning.
How Do Eye Doctors Diagnose Corneal Conditions?
Depending on your symptoms and risk factors, your eye doctor may perform one or more of these tests during your comprehensive eye examination:
Slit Lamp Examination

A slit lamp is a specialized microscope that directs a narrow beam of bright light onto your eye, allowing your eye doctor to examine the cornea’s structure in detail. During this painless examination, your eye doctor can detect changes in corneal thickness, surface irregularities, and any deposits or cloudiness that might indicate specific conditions.
Slit lamp examination is particularly valuable for diagnosing pterygium, corneal dystrophy, and corneal ulcers.
Fluorescein Staining
Fluorescein staining involves placing a special yellow dye into your eye to highlight areas of corneal damage or irregularity. The dye fills in any breaks or scratches in the corneal surface, making them visible under blue light examination.
This test is especially effective for diagnosing corneal abrasions and ulcers. During this test, your eye doctor will administer a small amount of fluorescein dye, then examine your eye under blue light.
Any damaged areas will appear bright green, clearly showing the extent and location of corneal problems.
Corneal Topography
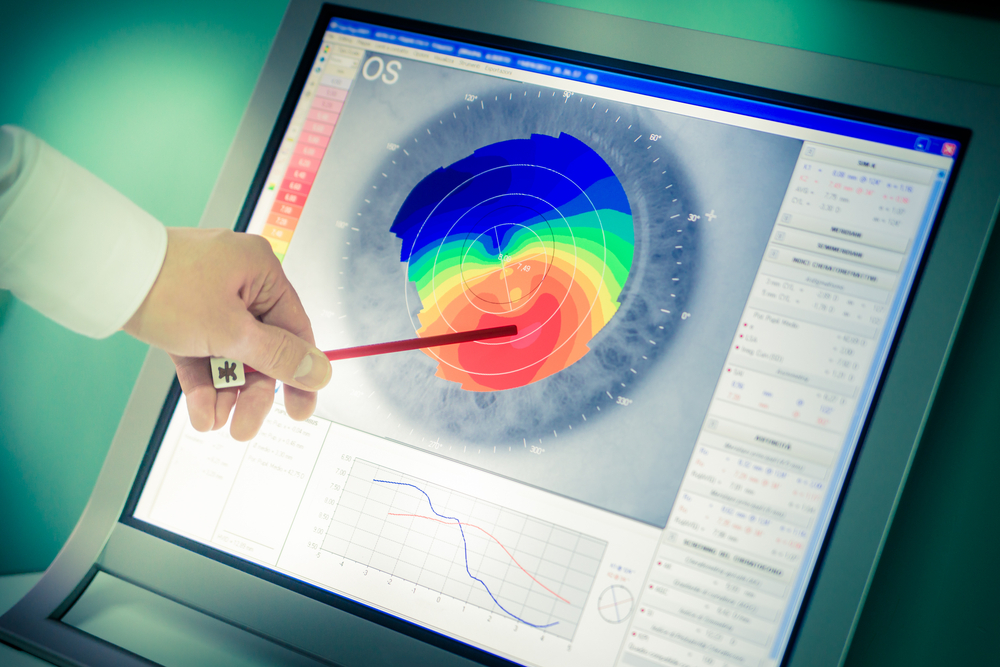
Corneal topography creates a detailed map of your cornea’s surface, measuring its curvature and elevation at thousands of points. This technology is particularly valuable for diagnosing keratoconus, a condition in which the cornea develops an irregular cone shape.
The topography system produces color-coded maps showing areas where the corneal surface is higher or lower than normal. These detailed measurements help your eye doctor track changes over time and plan appropriate treatments.
Corneal topography is also essential for monitoring corneal dystrophy progression and evaluating candidates for various corneal procedures.
Pachymetry
Pachymetry measures corneal thickness, which provides important information about corneal health and structure. This test utilizes ultrasound or optical technology to measure the thickness of various corneal layers.
Abnormal thickness measurements can indicate various conditions, including corneal dystrophies affecting deeper corneal layers. Pachymetry measurements are particularly important for diagnosing endothelial dystrophies and planning certain surgical procedures.
Optical Coherence Tomography (OCT)
While commonly used for retinal imaging, OCT technology also provides detailed cross-sectional images of the cornea. This non-invasive test uses light waves to create high-resolution images of corneal layers, helping identify structural abnormalities and measure corneal thickness with exceptional precision.
OCT imaging is particularly valuable for planning corneal treatments and monitoring healing after procedures. The technology allows your doctor to see deeper corneal layers that might not be visible during standard examination.
Keratometry

Keratometry measures the cornea’s curvature, which is particularly useful for diagnosing astigmatism and keratoconus. This test determines how steeply or flatly curved your cornea is, which affects how light focuses on your retina.
The measurement process involves looking into an instrument while your doctor takes readings from different meridians of your cornea. These readings help determine the degree of corneal irregularity and guide treatment decisions.
Culture and Laboratory Testing
When infection is suspected, your doctor may collect samples of eye discharge for laboratory analysis. A soft-tipped swab gently collects material from the eye’s surface, which is then sent to a laboratory for identification of bacteria, fungi, or other microorganisms causing keratitis or corneal ulcers.
In complex cases, corneal biopsy may be necessary. This involves taking a small tissue sample from the cornea for detailed pathological analysis.
While uncommon, corneal biopsy can provide a definitive diagnosis for certain types of corneal dystrophies or unusual infections.
How to Prepare for Your Eye Exam
Most corneal tests require minimal preparation. However, you should avoid wearing contact lenses for the period recommended by your eye doctor before the examination, as lenses can temporarily affect corneal shape and interfere with accurate measurements.
Bring a complete list of your medications, including eye drops, as some medications can affect corneal health. If you’ve experienced recent eye trauma or noticed sudden vision changes, seek immediate evaluation rather than waiting for a routine appointment.
These symptoms may indicate corneal problems requiring prompt diagnosis and treatment. Stay on top of your eye health by scheduling an appointment at Focal Point Vision in San Antonio, TX, today!
